Table of Contents
A basic evaluation includes a review of your visual and eye health problems and your family history. Your doctor will measure your vision using an eye chart to see how well you can read a line of letters that get smaller and may test the pupillary reaction by shining light through a specialized lens to determine if your pupils constrict correctly.
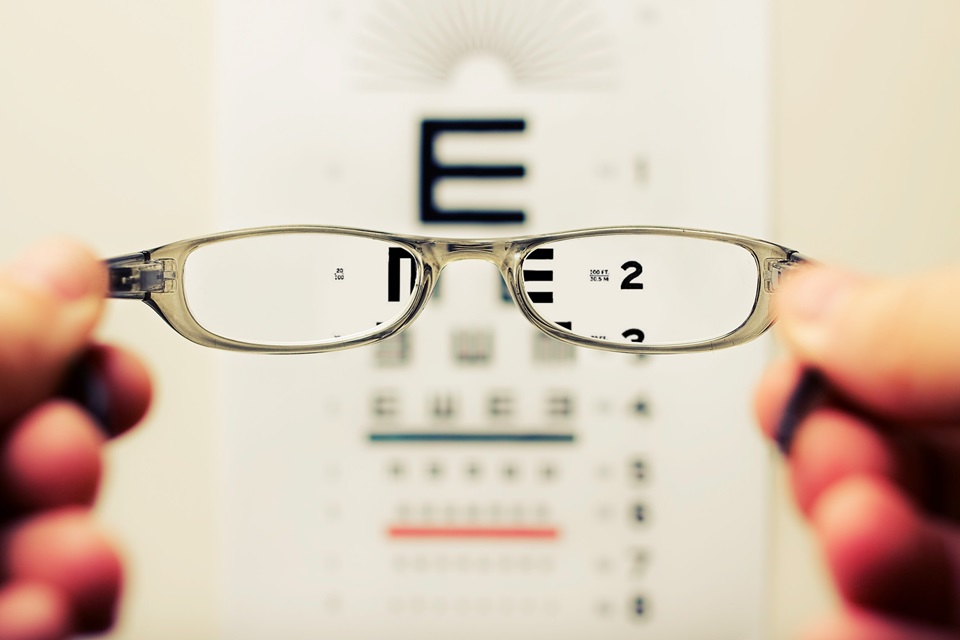
Visual Acuity Test
Whether you are having a routine eye evaluation test Arlington, WA or looking to get a new set of contact lenses, you’ll most likely have to take a visual acuity test. The test checks your ability to see clearly from a distance with and without corrective lenses.
Your doctor will ask you to remove your glasses and stand or sit 20 feet away from a chart with rows of letters or symbols that get smaller and smaller. Your goal is to read the lowest line on the chart that you can still see. Your results are then recorded as a fraction, the first number indicating how far you can see and the second number representing what you should be able to see with “normal” vision.
Refraction Test
Refraction tests examine the way light enters your eyes and focuses on your retina. It determines your optical prescription for eyeglasses or contact lenses. Your doctor shines a light in your eyes or uses a refractor machine, which looks like a big mask with holes for you to look through. They then cycle different lenses in front of you to find the ones that give you the best distance and up-close vision, a combination called your best-corrected visual acuity.
This test is typically given towards the end of a standard eye exam. Your doctor may also perform cycloplegic refraction, temporarily relaxing your focus muscles with eye drops to avoid children’s tendency to focus close up when they are supposed to be looking far away during the test.
Ocular Motility Test
To see a single clear image, your eyes must be able to change focus, move, and work together. Your eye care provider will look for problems that interfere with these functions, such as involuntary, rhythmic shaking (nystagmus).
They will assess your ocular motility by having you fixate on a distant target and then cover one eye. They will then observe the uncovered eye to see how it moves. If it deviates from its corresponding eye, it is called a phobia and can indicate a problem with your alignment.
They will also test your versions, the six directions your eyes can move in. If they are full and you don’t have complaints of double vision, your ocular motility assessment is complete.
Visual Field Test
The visual field test allows your eye care provider to check how much you can see up and down, left and right. This is important because glaucoma can sneak up on you, and it usually affects peripheral vision first. A visual field test can help your provider find early signs of glaucoma so they can start treatment.
There are a few different types of visual field tests, like the automated static perimetry test. In this, your doctor will cover one eye and then flash different lights at varying speeds on a perimeter screen. If you can’t see the flashing lights at certain time points during the test, you have a loss in that area of your visual field.
Other tests include the confrontation visual field test, where you look at a grid pattern and note which areas appear warped, blurry, or wavy. These tests can be used to monitor your glaucoma and are often covered by insurance.
Pupil Reaction Test
The pupils are a part of the iris and control how much light enters your eyes by shrinking or expanding. Your doctor can test how well your pupils respond to light by shining a bright flashlight into each eye and watching the response.
The first thing your doctor will look for is whether the pupil sizes are equal. A difference of more than a millimeter is abnormal and could indicate a condition affecting the brain, blood vessels, or nerves.
Next, your doctor will move the flashlight from eye to eye and watch how each pupil reacts. It should constrict quickly when the patient fixates on a near target, and it should be about the same size in each eye. This is called a direct pupillary light reflex and is documented using the acronym PERRLA.




No Comments